ACLS Instruction Videoshttps://www.acls.net/videos.htm
Also see these videos from our YouTube page at ACLSTrainingCenter
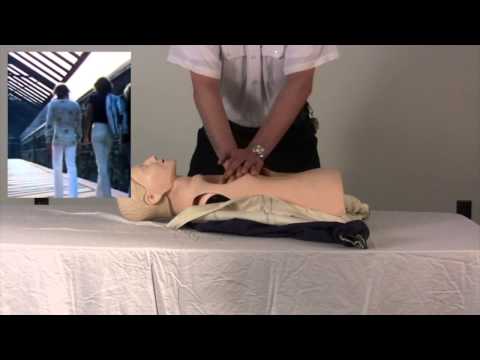
Basic Life Support Videos
Arrhythmia Interpretation / Monitor Tech
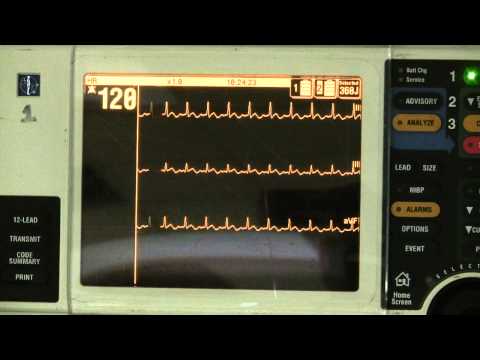
Normal Sinus Rhythm
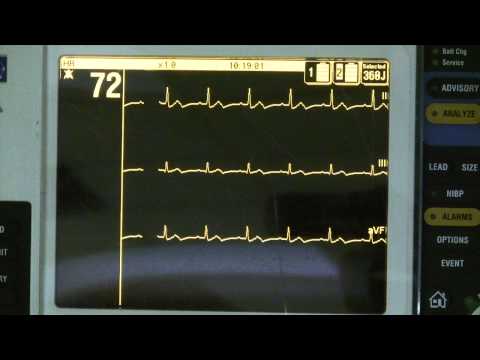
- Heart Rate = 60-100 beats per minute
- Regular Rhythm – slight irregularities are normal
- P waves precede each and every QRS complex
- The PR interval is between 0.10 and 0.20 seconds
- The QRS complex is within normal limits 0.08 - 0.12 seconds
- There is a QRS complex following each and every P wave
Atrial Fibrillation

Any rhythm that is grossly irregular and you cannot find P waves an accurate guess would be atrial fibrillation. A good way to tell the difference between atrial flutter and atrial fibrillation is that if you were asked to count the atrial rate it would be possible in atrial flutter because there are discernible flutter waves. It would not be possible to count an atrial rate in atrial fibrillation.
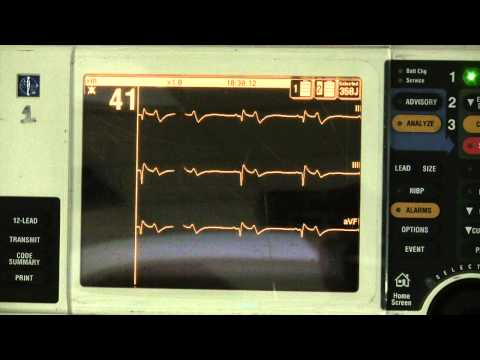
2nd Degree AV Block Mobitz I
Second Degree AV Block Mobitz I (Wenckebach). The only difference in this ECG strip and that of sinus rhythm is that the PR interval is longer. This is because it is taking longer for the impulse to travel from the SA node to the ventricles to cause depolarization. This AV block is usually benign although in patient’s with heart disease it can signal that more advanced AV blocks may be just around the corner.
2nd Degree AV Block Mobitz II
Second Degree AV Block Mobitz Type II. The key to this heart block is to remember that when the P wave is conducted all of the PR intervals are the same (vs. Type I in which they lengthen). This is an advanced heart block and the patient will always receive a permanent pacemaker prior to discharge if Mobitz II or Third Degree heart block is documented.
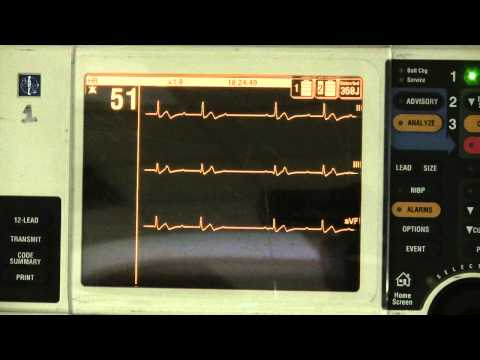
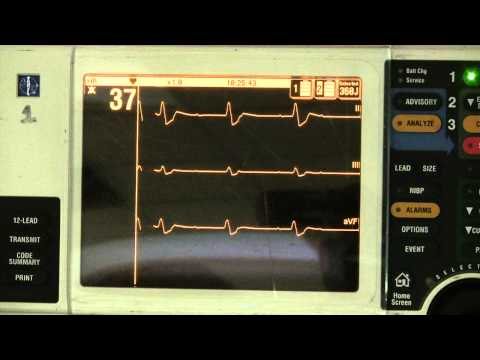
Sinus Bradycardia
You will note that the only difference between Normal Sinus Rhythm and Sinus Bradycardia is the heart rate. When you first learn how to interpret rhythms pay attention to the name (not the abbreviation) and it will give you a hint as to what it looks like. Rhythms are named first by the Pacemaker Site, then by the Ectopic Focus (if there is one) and then by the heart rate. For example, sinus bradycardia originates in the sinus node and the heart rate is less than 60 (bradycardia).
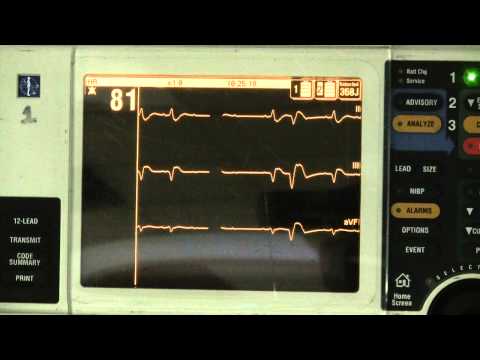
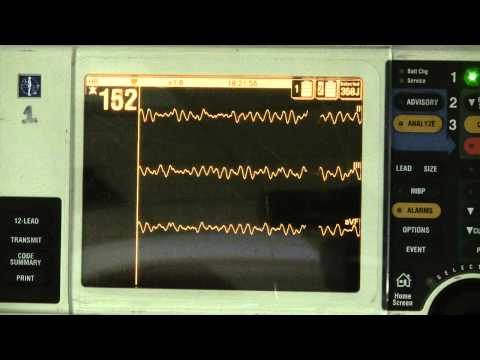
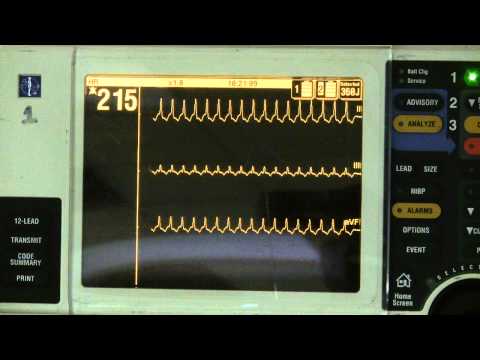
Sinus Tachycardia
Sinus Tachycardia originates in the sinus node and is faster than 100 beats per minute. Sinus tachycardia is always compensating for something. For example, if a patient is bleeding, the first thing the body will do is to increase the heart rate so that the blood that is left is pumped around faster.
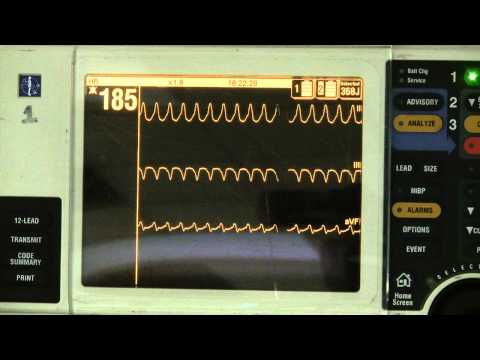
Atrial Flutter

Atrial flutter occurs when the atrium fires at such a fast rate that P waves become indiscernible. They instead blend together to become "flutter or F waves". In atrial flutter, the atria do not contract putting the patient at high risk to develop blood clots originating in the appendage of the atria.
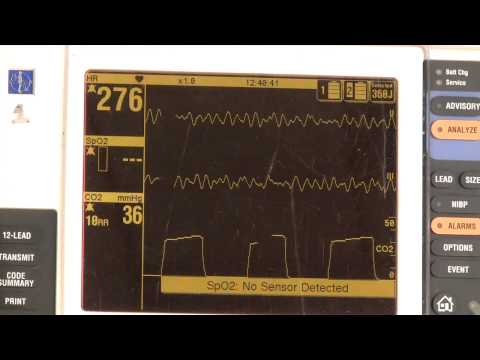
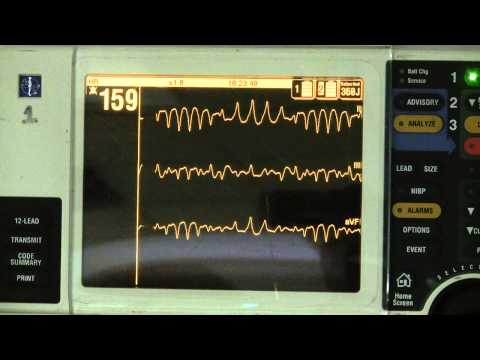
Ventricular Fibrillation
Ventricular fibrillation always represents a life threat. Hundreds or thousands of focuses are firing at the same time causing chaotic motion of the ventricle. If you were to look into the chest of a patient in ventricular fibrillation the heart would look as if you had Jello placed in a bowl and then bumped the bowl.








Comments